By: Kristen Lies, DPT
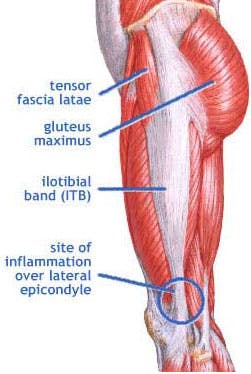
lliotibial (IT) band syndrome is a common overuse injury experienced by runners and active adults. It typically presents as a painful area on the outside of the knee that can be tender to touch and often increases in pain with activity. The IT band begins along the hip crest where the tensor fasciae latae and gluteus maximus muscles join to form this tendinous band. The band then tracks over the hip, down the outside of the leg, crosses the knee joint and inserts just past the knee joint line on the outside of the lower leg. Dysfunction of this IT band often arises from poor biomechanics during repetitive activities such as running, cycling, etc. for various reasons such as muscle imbalances and/or leg length discrepancies.
One example of poor biomechanics that can contribute to IT band syndrome is described as a valgus knee position that people sometimes experience during the weight bearing phase of running. This valgus angle describes a position of the knee that is more medial (or towards the midline of the body) than the hip and foot during weight bearing. This position of the knee relative to the hip during repetitive activities such as running causes significant stress and strain to the IT band. This strain multiplied by the thousands of times that individuals will take a step can lead to undue muscle tension and tightness, known as myofascial restrictions. These myofascial restrictions present as palpable taught muscle bands or even knots known as trigger points that can also be tender to touch. They can occur anywhere along the length of the IT band and cause tension and tightness resulting in strain, inflammation and pain where the tendon inserts into the bone just past the knee.
Once an individual develops symptoms related to IT band syndrome, it is helpful to see a Physical Therapist for evaluation to decipher what might be their specific impairment leading to poor biomechanics and this particular overuse injury. One common cause of the valgus knee position during weight bearing is weakness present in the muscles located on the outside of the hip. When these muscles function properly, they aid in maintaining a neutral knee position while an individual weight bears on one leg. If there is weakness present, these muscles will stretch and allow the knee to translate medially (or towards the midline of the body) leading to the valgus knee position. Another cause of this valgus knee position can be located on the opposite end of the chain, the foot. If a person has more of an unstable foot, where the arch collapses during weight bearing, this causes the lower leg, and thus the knee, to translate into the valgus leg position when bearing weight on one leg. If either or these factors are found to be causes in the case of an individuals IT band syndrome, the physical therapist can direct the individual with appropriate exercises to help strengthen and stabilize where necessary to reduce strain on the knee.
In addition to addressing the biomechanical causes related to muscle imbalances, it is imperative to address the myofascial restrictions present in the IT band in order to increase soft tissue extensibility, reduce inflammation, and decrease pain. Soft tissue restrictions will be addressed through various techniques such as foam rolling, soft tissue massage, and/or dry needling as well as therapist instructed stretches to most appropriately address the individual’s restrictions. Dry needling is a procedure where fine gauge solid filament needles are inserted into the symptomatic tissue in order to stimulate the body’s natural response of healing and to release or deactivate active trigger points. Dry needling is now being offered at all of our Professional Rehabilitation Services Offices.
If an individual suspects they have symptoms related to IT band pain syndrome, they would benefit from being evaluated by a physical therapist to decipher their specific impairments contributing to the dysfunction. Then, through soft tissue technique and the instruction of proper exercise, they can eliminate their current pain symptoms as well as learn appropriate exercises to maintain in order to ensure their symptoms do not return as they return to their sport and continue to lead an active lifestyle.
