Dr. Richard DeFalco, DPT, OCS, CSCS, CWcHP, Cert. DN
One of the more common areas of injury we treat in our outpatient physical therapy setting is the knee. In this article we will discuss two types of knee pain commonly seen in athletic populations.
The first is patellofemoral dysfunction (PFD). This type of knee pain arises from a dysfunctional movement (maltracking) of the patella (kneecap) within the femoral groove it moves in. In other words the knee cap is moving incorrectly causing repetitive micro trauma. The pain in most cases is described as a dull ache in the front of the knee, behind or around the area of your patella. It is commonly seen more in females than in males due mainly to anatomical predisposition. Pain is usually reported with activity, stair negotiation, and rising from a prolonged seated position. It is also commonly seen with repetitive landing forces and improper equipment set-up in runners and cyclists respectively. Overall, during these activities you are eccentrically loading the joint and there is a dramatic increase in joint pressure, ranging from 3-20x your bodyweight. These pressures combined with a maltracking patella leads to a myriad of problems and subsequent pain.
PFD can be due to anatomical predisposition, muscular imbalances, decreased flexibility, limited joint mobility, training errors, or a selected combination. An important concept to remember is that the lower extremity (i.e., your leg) is a linkage system that includes a series of joints, beginning at the foot and extending into the trunk, which in combination make possible the transmission of forces during running, jumping, kicking, throwing, cycling, and other forms of activity. Dysfunction in any area of this linkage system may result in dysfunction and subsequent pain in another area. This means that your knee pain may be a result of a problem originating in your hip or your foot/ankle. More importantly, there is no “one size fits all” approach to treating this condition and a thorough physical therapy evaluation will detect if there are specific components contributing to your problem. An individualized and evidence based treatment approach should be initiated.
Another common knee condition that is commonly treated in the outpatient physical therapy setting is patellar tendinopathy (sometimes referred to as jumpers’ knee), which is a generic term used to describe conditions that affect the patellar tendon. Patellar tendinopathy occurs more frequently in skeletally mature adolescents or adults, ranging from ages 16-40 years, though not solely limited to this population. Recent studies show equal occurrences in both males and females. Usually the condition is further described or diagnosed as a tendonitis or tendinosis, which is determined based on the stage of the injury and symptoms present. Acute tendinitis involves an active inflammatory process, often occurring following an injury or training errors, which if treated, properly heals in 3-6 wks. In contrast, chronic patellar tendinosis manifests itself after 6 wks-3 months and beyond as degenerative changes occur in the tendon. At this stage there is a disorganized arrangement of tendon fibers, though there are no inflammatory cells present. Pain is reported in the anterior aspect of the knee, below the patella (knee cap), and usually occurs with activity/exercise, ceasing with rest. If left untreated and causative factors are not addressed, there exists the possibility of progressive weakening and subsequent tendon rupture. A correct diagnosis is essential, in that there are differences in the treatment approach for both tendonitis and tendinosis, and a poor outcome, may be the result of incorrect treatment design, not a failure to respond to conservative treatment. As above, these conditions can be caused by in part or whole by anatomical predisposition, muscular imbalances, decreased flexibility, and training errors and we must consider that the causative factor for your knee pain may, in fact, be somewhere else in the linkage system.
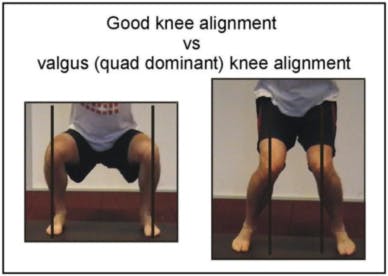
Some of the more effective treatment approaches include corrective exercise to address the suspected muscle imbalances, patellofemoral taping to unload irritated tissues and/or reposition structures, manual therapy to release any restricted tissues or joints, and recommendation of orthotics/bracing to reposition or offload certain areas. See Figures 1-3 that show improper alignment of the lower extremity as well as taping techniques to reduce stress on the patellofemoral joint.
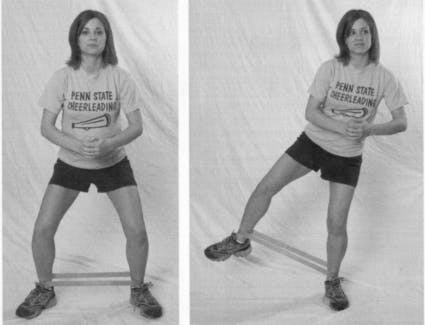
To offset some of these problems, a good starting point would be wise to implement of strengthening program that targets the muscles of the hip, specifically your hip abductors and external rotators. See Figures 4-5.
Dr. Richard DeFalco is a physical therapist with Professional Rehabilitation Services in Myrtle Beach. He is a Board Certified Orthopedic Specialist as well as a Certified Strength and Conditioning Specialist. He treats patients of all ages and activity levels that suffer with neuromusculoskeletal disorders. He can be contacted at (843) 839-1300 for further information or to schedule a Free 15 Minute Consultation. Visit www.prsrehabservices.com for more information.